Sleep is a mega daily challenge for many autistic children and their families. Ongoing scientific research in this field seem to indicate a challenge with melatonin levels among the autistic population. That said, sleep problems can have a severe impact not just for the autistic child but for the whole family. Many times, mothers stay up the whole night trying to settle the child for bedtime. The child may also have issues of night waking and then not settle at all for the rest of the night. All this struggle can terribly wear down a mother and contribute to extremely high levels of maternal stress. It also impacts a child’s behaviour, cognitive performance and attendance in school.
Restful and adequate sleep is the foundation for optimal learning, cognitive development occupational performance, participation, and engagement in daily life. Lack of sleep impacts attention, concentration, memory and can cause stress, muscle tension, fatigue, body aches and overall health problems. Sleep patterns of autistic children have to monitored, observed and plans have to be prepared for their sleep hygiene. Sleep needs of parents and carers are also high priority. Holistic life can be led only with a good sleep cycle.
Sleep insufficiency means not only lack of restorative sleep, it means deprivation. It can lead to chronic diseases such as hypertension (in carers & parents), diabetes, depression, and obesity, along with early mortality, and reduced quality of life and productivity [CDC (2015): Insufficient sleep is a public health concern]. Sleep problems must be viewed from the perspective of health maintenance and promotion.
Those children reporting unresolved, chronic, or potentially serious sleep problems as also their carers must get help with intervention strategies and consultations with Neurologists and Paediatricians. Many times lack of sleep is a sign of an underlying health condition (eg: gut issues like IBS, neurological condition like Epilepsy) and that needs to be treated.
Chris Hoyle who has been running The Sleep Clinic for the past 14 years and a service called Sleep Tight Trafford, in Trafford UK, says, a lot of parents are told that sleep problems are part and parcel of autism. Not so. There is always something that can be done for making sleep better. Hoyle advises screening children early for sleep difficulties and making the child understand bedtime routines and incorporating changes to the child’s bedroom sleeping environment.
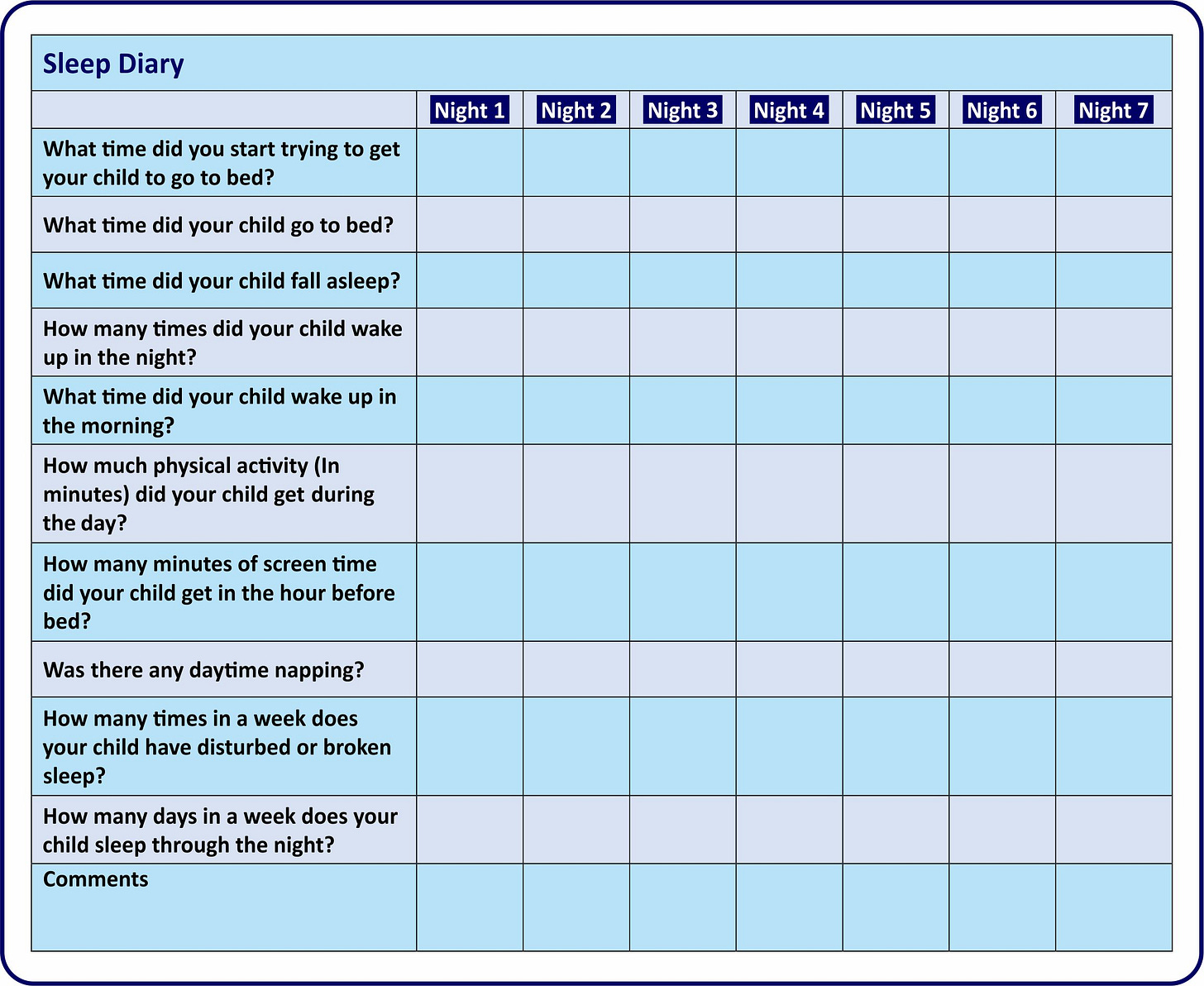
Parents need help with creating a personalized sleep plan for their child, this is really very important. It involves collecting data on several parameters so as to arrive at the child’s sleep history and then create the resources for a healthy sleep schedule.
For an advanced reading of sleep science and how it can make people healthier and smarter, Dr Matthew Walker’s international bestseller, ‘Why we Sleep’, maybe referred to.
Intervention Framework
Occupational Therapy frameworks handle sleep issues for children and their families. Occupational Therapists (OTs) use knowledge of sleep physiology, sleep disorders to evaluate and address the ramifications of sleep disorders on performance and participation. OTs may use sleep promotion practices to implement intervention strategies.
OT practitioners must first catalogue the impact of sleep deprivation on the family unit and the child’s and caregiver ability to function effectively during the day. They can then aid families to systematically trial changes in bedtime routines, habits, and patterns. OTs carry out detailed sensory profile assessment. These need to be dovetailed. For example, by noting sensory seeking or sensory avoiding behaviours, changes can be made to the type of night clothing and bedding. There are many factors involved here. A child may prefer a full shirt to a half one, may prefer a lighter blanket to a heavier one, the child may prefer a duvet to a sheet. A child maybe sensitive to street lights and require blackout curtains.
Managing the physical environment pre-sleep is also a major focus area. Parents need to be trained for observation skills and for anticipating reactions to changes in clothing, toys, diet or family schedules. The specific areas where most parents need advice are: adjusting lighting, reducing noise, bed positioning, bedding management, clothing, room temperature/cooling, nocturnal toileting also, so that bed-wetting issues can be removed.
Calming activities and routines need to be considered to facilitate sleep. Bedtime and wake up time routines are usually stabilised over time. It does not happen in a day or week. And it needs consistent practice. Parents need to work on setting a regular bedtime, limit screentime before going to sleep and keep distractive devices likes tablets out of the bedroom and mobile phones in silent/switched off mode. Visuals or Picture poster maybe used to cue and kick-off this process for autistic children who are minimally verbal or non-verbal.
According to the Autism Speaks sleep toolkit, some children may not even relate to a visual schedule that uses photos, images or icons, then an object board maybe created using objects involved before bedtime preparation like toothbrush for brushing, hairbrush for combing, nightclothes, blanket. What is important is going through the same steps each night and adhering to the routine. Children are also taught through cognitive behavioral restructuring techniques, such as leaving the bedroom if awake and returning only when sleepy. Meaningless plonking on the bed should be discouraged. Through daily continuous practice children can be taught self-management.
The preferred sleep hygiene format as a practice is no daytime napping. However, a child may have some health condition like epilepsy and may need short daytime rest breaks. OT practitioners need to consider such conditions while developing individualized sleep routines.
Daytime activity programs of exercise improve the mood of the child and work the muscles. Lack of structured physical activity is linked with sleep disturbances. Physical Education plus environmental elements improve sleep latency and enhance quality of sleep.
After implementing the intervention, OTs need to evaluate children in the area of sleep latency: how long it takes to fall asleep - this is typically fewer than 30 minutes for someone without a sleep disorder. Information needs to be gathered on sleep duration: the number of hours of sleep and sleep maintenance.
OTs also need to check if sleep dysfunction persists despite behavioural and environmental changes.
In Conclusion
Sleep health is a physical, emotional wellbeing and work productivity strategy for an autistic child. Lack of this discipline results in daytime sleepiness impacting school and life events. It can overly tire the parent undertaking caregiving responsibilities or the caregiving assistant. For the child there can be additional burdens related to disturbances in balance, vision, strength, sensory systems, psycho-emotional status, anxiety, and stress and impact on food intake. Therefore, it is necessary to research and identify the appropriate interventions to improve sleep quality for children and thereby decrease parental stress load. In this OTs have a pivotal role in formulating sensory strategies and environmental modifications.